
(Photo: Fiona Goodall/Getty Images)
Ask your doctor about methamphetamine. It’s not a phrase you’ll ever hear on TV or the radio, but here’s a secret: Meth is an incredible medicine. Even the Drug Enforcement Administration admits it, and doctors are known to prescribe it for narcolepsy, obesity, and ADHD. Historically, meth has been used to reverse barbiturate overdoses and even raise blood pressure during surgery. Some preliminary research suggests that meth can be neuroprotective against stroke and traumatic brain injury, even stimulating the growth of brain cells.
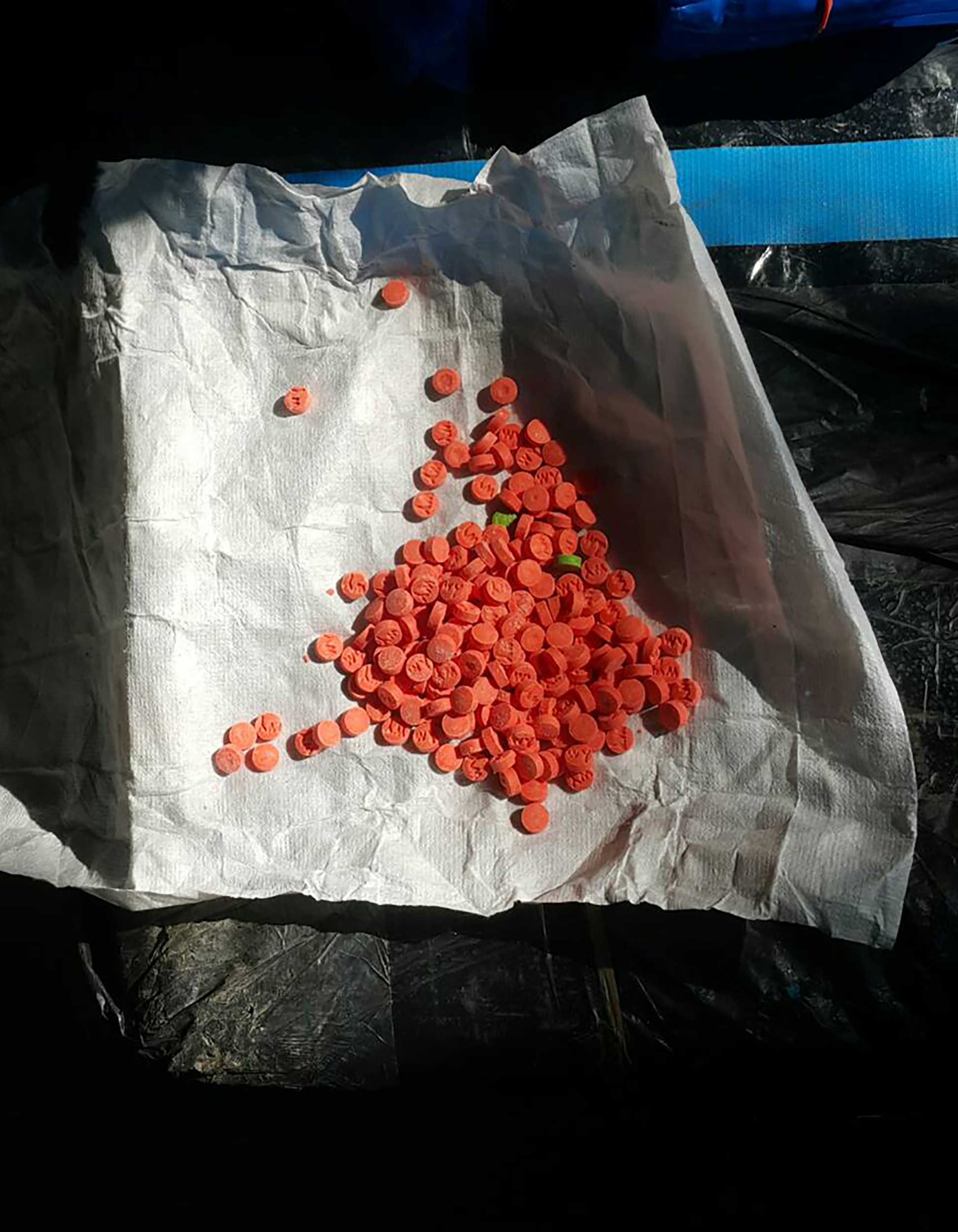
Yet we’re constantly warned never to try meth—”not even once,” goes the refrain—or it will instantly cause addiction and ruin your life. Before fentanyl was the demon drug du jour, meth was seen as the worst, most destructive, most evil chemical you could find on the streets. Even of late, if you ask the New York Times or NBC, you’ll learn that meth, “the forgotten killer,” is back with a “vengeance.” Other outlets, from Rolling Stone to CNN to The Daily Beast, have raised the alarm about meth use in the context of the opioid overdose crisis.
Stimulant-related deaths are indeed on the rise in North America—in some regions, meth is even more prevalent than heroin. Surveying drug overdoses in America from 1979 through 2016, researchers wrote in Science in September of 2018 that “Methamphetamine deaths have increased most dramatically in the western and southwestern United States.”
Meth poisonings accounted for an estimated 14,845 hospitalizations in 2015, according to the Centers for Disease Control and Prevention (CDC), and another 15,808 emergency room visits. In 2016, around 7,500 people died from overdosing on stimulants, including meth. If you ask most people, including policymakers, you’ll hear that meth is a scourge that can do no good.
But if you’ve ever used something like Vicks VapoInhaler, you’ve experienced the healing benefits of meth firsthand. That’s because the over-the-counter nasal decongestant contains levomethamphetamine, the levorotary form—or “mirror image“—of the same stuff from Breaking Bad. Procter & Gamble tries to obscure this fact by spelling the active ingredient “levmetamfetamine.” Selegiline, a drug for treating Parkinson’s and Alzheimer’s diseases, also metabolizes into levomethamphetamine.
There is a significant difference between these two opposing molecules. D-methamphetamine is what generally appears on the street—although it’s often cut with other chemicals—whereas l-meth provides a less addictive, shorter-lived high that is less desirable among drug users. But people can and do use it recreationally. Abuse is rare, however, in part because the high is shitty, but also because d-meth is so widely available. It’s easier to buy a more powerful form of the drug on the street than it is to try to extract it from over-the-counter medications.
Other Americans are prescribed actual, pure meth by their doctors. It happens less frequently these days, but in ADHD, obesity, or narcolepsy cases where nothing else has worked, a drug called Desoxyn (methamphetamine hydrochloride) can sometimes help. It can even be prescribed to children as young as seven.
It’s important to make these distinctions. Meth didn’t make a “comeback”; it never left. It can’t return with a “vengeance” and it can’t be “evil” because we’re talking about a chemical compound here. It has no personality, no feelings, no intentions.
Thus it does a disservice to science and to medicine, as well as to the people who use these drugs responsibly, to treat a molecule with dualistic properties purely as a poison. And as recent research has shown, we’re still uncovering some of the potential therapeutic benefits of methamphetamine. Confronting the stigma associated with meth and highlighting its benefits can better inform drug policy and addiction treatment.
‘It’s Just a Stimulant, Like Any Other Stimulant’
For Jordan*, the meth he’s prescribed works better against his ADHD with fewer side effects than the Adderall he’d been on for 20 years. About five years ago, Jordan asked his doctor if he could try methamphetamine. The doc said sure.
“The first time I brought it to the pharmacy, the pharmacist actually said to me, ‘Oh, your doctor wrote this prescription wrong, this is the stuff that they make in meth labs,'” Jordan tells me by phone. “I told him to type ‘Desoxyn’ into the computer, and he did. He kind of backtracked, [but] he obviously had no idea.”
Jordan, a middle-aged man from North Carolina who works in clinical research, now switches every three months between Adderall and Desoxyn to prevent building a tolerance to either stimulant.
Methamphetamine and amphetamine (one of the active ingredients in Adderall) are almost identical chemicals. The main difference between the two is the addition of a second methyl group to methamphetamine’s chemical structure. This addition makes meth more lipid-soluble, allowing for easier access across the blood-brain barrier. Meth is therefore not only more potent, but also longer-lasting.
“The medications have definitely been important for me, to be productive, to be successful, not just at work but also in my personal life,” Jordan says. “I’ve been on the medications for years, but I can take Adderall or methamphetamine and take a nap afterwards. I don’t have any noticeable side effects.”
Jordan also doesn’t feel “high” from the doses he takes—approximately 10 to 15 milligrams of meth per day. Doses at this level are well tolerated by most people. It’s very difficult to estimate the typical dosages of illicit meth taken on the street, but they are generally many times higher and taken every couple of hours. Further, the route of administration—typically, users smoke or inject illicit meth—allows for more of the drug to enter the bloodstream than taking a prescription pill.
At high doses, meth gives a rush of euphoria, boosting attention span, zapping fatigue, and decreasing appetite. Intense sexual arousal, talkativeness, and rapid thought patterns are also common. Body temperature and heart rate shoot up, which can cause irregular heartbeat, increasing the risk of seizures. If taken repeatedly over long periods, street meth can be highly neurotoxic, inducing paranoia and psychosis.
But illicit meth is also often used to self-medicate, according to Mark Willenbring, an addiction psychiatrist from St. Paul, Minnesota, with over 30 years of practice treating substance-use disorders. In Willenbring’s experience, most of his patients who use illegal meth are treating undiagnosed ADHD.
“There’s a high degree of comorbidity between substance-use disorders and ADD,” Willenbring says. “They used meth for years in a controlled way, they never over-used it, they just used enough to get an effect, and then they stopped. One misconception is that it’s always very addictive.”
With most people who are addicted to meth, Willenbring says, you can’t tell it just by looking at them. Carl Hart, a neuroscientist in Columbia University’s Department of Psychology, agrees that the image of a snarling meth addict with bad teeth is a false stereotype. The dental damage so prevalent in anti-drug propaganda, he says, is more likely due to poor nutrition and lack of sleep—not to the drug. “There is no empirical evidence to support the claim that methamphetamine causes physical deformities,” Hart wrote in a 2014 co-authored report.
“It’s just a stimulant, like any other stimulant,” Willenbring says. “It’s a marketing issue.”
Part of the reason Jordan asked to try Desoxyn in the first place was to see if he’d develop any of the “stereotypical meth addict problems,” as he puts it. He hasn’t.
“Those of us that know the reality have a responsibility to say, ‘Hey, not that shooting up meth isn’t bad, but the chemical itself isn’t bad,'” Jordan says. “It’s just misuse of the chemical that’s bad.”
For Joan*, a 66-year-old grandmother living off the grid in northern Georgia, Desoxyn makes her feel normal. “Not high, not hyped up, just normal,” she tells me. She’s been taking prescription meth since 2006, but first tried many other ADHD meds, such as Ritalin and Concerta, with poor results. But Desoxyn has not only helped her socialize, manage bills, and finish her master’s degree in social work; it’s also helped with Joan’s depression and self-esteem.
“The only downside is the cost,” she says. “It’s one of the oldest drugs on the market, but even generic, it is outrageously expensive.”
Still, meth isn’t for everyone, of course. Kevin*, a 31-year-old artist from the Midwest, was first prescribed Desoxyn at age 15 to treat extreme fatigue and trouble focusing. But misdiagnosed mental-health issues—his doctors thought he had bipolar disorder, when in fact he had post-traumatic stress from childhood abuse—led to worsening symptoms.
“Being able to just take a bunch of pills that made the exhaustion go away for a while felt like a blessing, but it was just a Band-Aid on the problem,” Kevin says. “I became completely dependent upon Desoxyn to function, and any lapse in taking my dose would result in a terrible energy crash.”
“In retrospect, my neurologist at the time would have done well to consider the effects of intense stimulants on someone already prone to mania, insomnia, and hallucinations,” he says. “I think Desoxyn has its merits as part of a treatment plan for attentive disorders, but that’s the thing—it needs to be part of a larger understanding of how and why it might have a negative impact upon the patient’s overall health, and should remain closely monitored throughout.”
!["Stigma is the lens [through] which we see all drug issues. It keeps us from making the best decisions. It is fear-based, not rational, not creative. Because of stigma, we have not fully addressed the opioid crisis."](https://psmag.com/wp-content/uploads/2024/07/gettyimages-1024888414-1024x683.jpg)
How Meth Can Treat Brain Injury—and Much More
Street doses of meth can be extremely damaging to your health. The purity of such drugs is often unknown, and repeated, high doses of meth have been proven to be neurotoxic. But in low, pharmaceutical-grade doses, meth may actually repair and protect the brain in certain circumstances.
This was first discovered in 2008, when researchers at Queen’s Medical Center Neuroscience Institute in Honolulu, Hawaii, analyzed five years of data on traumatic head injuries. They unexpectedly found that patients who tested positive for methamphetamine were significantly less likely to die from the injuries. The authors suggested that meth could have neuroprotective benefits.
To learn more, in 2011, a different team from the University of Montana applied meth to slices of rat brain that had been damaged to resemble the brains of stroke victims. Then they induced strokes in living rats, using a method called embolic MCAO, and injected them with methamphetamine. At low doses, the meth gave better behavioral outcomes and even reduced brain-cell death. At high doses, the meth made outcomes worse.
Because meth stimulates the flow of important neurotransmitters—dopamine, serotonin, and norepinephrine—the Montana researchers theorized that methamphetamine may provide neuroprotection through multiple pathways. David Poulsen, one of the researchers involved, says this was a “serendipitous discovery.”
“So we decided, well, if it worked in stroke, it’s probably going to work really well in traumatic brain injury,” says Poulsen, now a neurosurgeon at the University of Buffalo who specializes in treatments for protecting the brain after severe damage.
Traumatic brain injury, or TBI, occurs after a violent smash to the skull. Its consequences include concussions on the mild end and coma or death on the severe end. TBI kills around 50,000 Americans annually, according to the CDC, while about 2.8 million of us visit the emergency room for TBI-related injuries every year. There is currently no Food and Drug Administration-approved treatment for TBI.
So, Paulson and his team reasoned, if meth can already be prescribed for children, why not to adults with TBI?
To test the proposition, Poulsen and colleagues gave TBI to rats. Giving an animal brain trauma isn’t easy, but for more than two decades, there’s been a trick called the rat lateral fluid percussion injury model: Simply cut a hole in the skull of a rat and apply water pressure to the brain.
About half the rodents—19 male Wistar rats—were given this treatment, and eight of these were then given meth. The rats given meth performed better at a task called the Morris water maze, a widely used experiment that involves plopping a rat into a pool of water with a hidden platform. By tracking how long it takes the rodent to find the platform, scientists can measure many different aspects of cognitive function.
“By the third day of training, there were no statistically significant differences between the uninjured control rats and the injured rats that had been treated with methamphetamine,” Poulsen and his colleagues wrote.
But the team also found that low doses of meth were protecting immature neurons, while also promoting the birth of new brain cells that are important for learning and memory. The same was also true for rats that were given meth, but not injured.
“We see not just little, but very significant improvements in cognition and behavior,” Poulsen says. “Their memories improved, functional behavior is improved…. It’s not a trivial difference.”
“In light of the fact that low-dose methamphetamine is FDA-approved for use in juveniles and adults, we see no valid reason why it cannot be utilized in human clinical trials for stroke and TBI,” Poulsen and colleagues concluded in 2016.
But those clinical trials, considered the gold standard for testing medication, have yet to materialize, even while a 2018 retrospective study found similar results to the Hawaiian neuroscience report: Out of 304 patients with TBI, those who also tested positive for meth had better recovery results than those who did not. “The potential neuroprotective role of meth and other similar substances cannot be ignored,” the authors wrote in Clinical Neurology and Neurosurgery last July.
There are limited conclusions that we can draw about these rodent and retrospective studies, and it’s probably unlikely that nurses will soon start giving meth to people who have cracked their skulls. Still, a wide variety of stimulant therapies for TBI is being explored, with positive results. These include trials with modafinil, a narcolepsy drug; amantadine, a Parkinson’s drug; and dextroamphetamine, one of the components of Adderall. But there’s still no indication of a single clinical trial for methamphetamine for TBI registered with the National Institutes of Health.
Methylphenidate, also known as Ritalin, seems to be the stimulant most popular in these trials. For example, in 2004, researchers at Drucker Brain Injury Center at MossRehab Hospital in Pennsylvania gave methylphenidate, better known as Ritalin, to 34 patients with moderate to severe TBI. They reported significant improvements in information processing and attention.
Twelve years later, in Gothenburg, Sweden, another 30 patients suffering from prolonged fatigue following TBI were given methylphenidate and observed for six months. They also showed improved cognitive function and reduced fatigue. But a 2016 meta-analysis of 10 controlled trials found the main benefit of giving methylphenidate for TBI was increased attention, “whereas no notable benefit was observed in the facilitation of memory or processing speed,” the authors wrote. They encouraged more research into appropriate dosages and length of prescription.
Birgitta Johansson, a neuroscientist at the University of Gothenburg and lead author of the Swedish study, suggests caution whenever treating someone with a brain injury. “With methylphenidate, it is important to be aware about possible side effects, [such] as increased blood pressure and heart rate and also risk of anxiety,” she says. “It is always very important to prescribe medication with care and follow the patient carefully.”
But the reason meth isn’t studied more rigorously—for TBI, for Alzheimer’s and Parkinson’s, for stroke—could also come down to money. Methamphetamine is off-patent, meaning there may be less financial incentive for pharmaceutical companies to explore the drug’s potential uses. Consider Vyvanse, a drug first marketed in 2007, with a new formulation introduced in 2017, that racked up $2.1 billion in sales in 2017. Desoxyn, which is sold by three companies, only earned about $9.3 million in 2009.
While Methamphetamine may not be widely recognized as medicine, it clearly has potential to heal as well as harm. Recognizing the duality of meth is arguably all the more essential in the face of a rising stimulant overdose crisis.
“Stigma regarding any substance use or substance use disorder is counterproductive,” says Dan Ciccarone, professor of family medicine at the University of California–San Francisco. He says the overdose crisis is shifting from opioids to stimulants and that we are not prepared for the next wave. “Stigma is the lens [through] which we see all drug issues. It keeps us from making the best decisions. It is fear-based, not rational, not creative. Because of stigma, we have not fully addressed the opioid crisis.”
That stigma remains a major hurdle, and until doctors and public-health officials counteract this kind of messaging, it seems unlikely that a multinational pharmaceutical company would risk marketing a substance only believed to be toxic and deadly.
“Everything will kill you, if you take enough of it,” Poulsen says. “Some things don’t require a lot to do that. Meth is one of those things. But just like any drug, the difference between a poison and a cure is the dose.”
*These names have been changed.





