Much of the public debate around the version of the American Health Care Act passed by the House of Representatives earlier this month has centered on the so-called “MacArthur amendment.” A last-minute addition intended to attract support from Tea Party congressmen, the amendment would allow states to obtain waivers from Obamacare’s community ratings provision. While GOP leadership has maintained that the bill provides adequate protections for those with pre-existing health conditions, many health policy experts have raised concerns that the $128 billion included in the AHCA for states to set up high-risk pools is woefully inadequate.
Last week, Urban Institute researchers Linda Blumberg, Matthew Buettgens, and John Holahan released a paper estimating just how much money it would require to fund high-risk pools for people with pre-existing conditions. Their findings suggest that the AHCA falls far short of the funding levels needed to provide even stingy coverage to those with pre-existing conditions.
The researchers estimated funding needs under several different scenarios for patients suffering from nine different conditions—diabetes, asthma, coronary heart disease, angina, heart attack, other heart disease, stroke, emphysema, and arthritis. Specifically, they varied eligibility rules, allowing for both narrower eligibility (covering only those who would experience high claims under standard coverage) and broader eligibility (including those with chronic conditions). They also varied coverage and subsidy levels, estimating funding requirements for a coverage and subsidy level similar to the Affordable Care Act (i.e. fairly generous) and funding requirements for a coverage and subsidy level “more typical of traditional high-risk pools” (i.e. stingy coverage, no income-related premium subsidies).
The chart below, from the report, illustrates their findings:
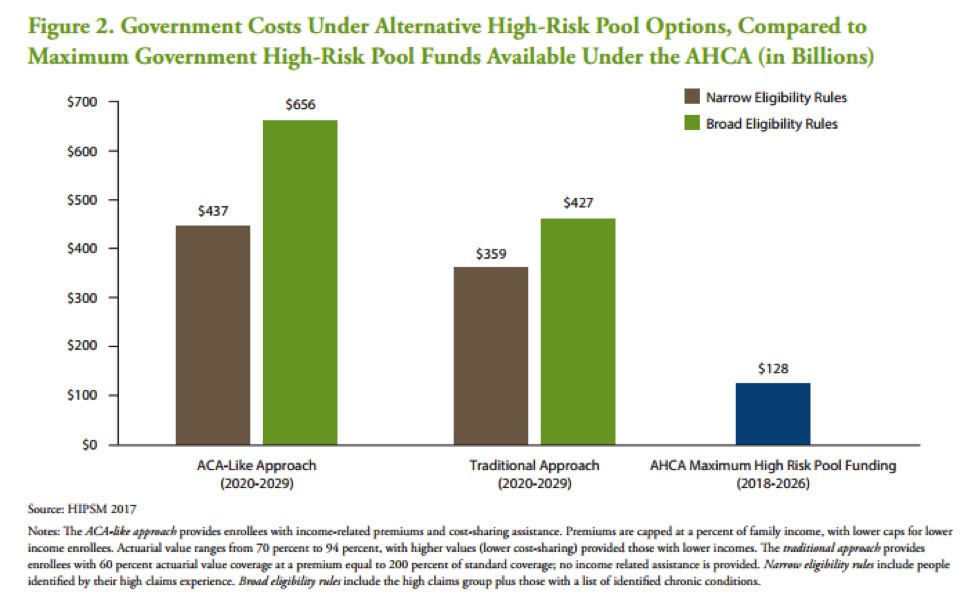
Under none of the scenarios is $128 billion enough to fund high-risk pools for everyone in need. Even under the cheapest scenario—narrow eligibility rules, stingy coverage—the cost of funding the pools over 10 years would run to approximately $359 billion. And $359 billion doesn’t exactly buy great outcomes for patients in those pools: The researchers predict many will have to forgo insurance entirely (they estimate only 19 to 26 percent of those eligible will enroll) and any who do enroll will likely face high out-of-pocket costs. They predict the median enrollee under the “traditional” design will spend between 35 and 41 percent of their income on health-care costs.
The AHCA falls far short of the funding levels needed to provide even stingy coverage to those with pre-existing conditions.
“This least expensive approach leads to the lowest enrollment, the highest financial burdens for high-risk pool enrollees, and the highest number of uninsured, yet it would cost more than double the government funds under consideration for such a program,” Blumberg and her co-authors conclude.
It’s not all bad news for fans of high-risk pools: The researchers predict that patients would fare much better under the more generous, ACA-like approach, spending only 8 to 10 percent of their income on health care and enrolling at higher rates. The problem is that such an approach comes with a much higher price tag—$437 to $656 billion.
The American Health Care Act is in the hands of the Senate now, and quite a few moderate Republican Senators have expressed concerns about the bill’s current design with respect to pre-existing conditions. Some of them might want to take a look at this report.



