Socio-economic class affects the way children are prescribed pills—and not at all in the way you’d expect.
By Malcolm Harris
(Photo: Michael David/Flickr)
The stereotypical medicated kid in America is wealthy and spoiled and retains a psychiatrist to guarantee him extra time on tests or to help process the emotional fallout of being neglected by high-powered working parents. In this formulation, rich kids have psychological problems, and poor kids have real problems. But the stereotype isn’t accurate; the correlation is, in fact, the opposite. Children in poor families are significantly more likely to be diagnosed with emotional and behavioral problems and to be prescribed medication. Our national understanding of youth and mental health starts with an important mistake.
Commentators posit a variety of logical, common-sense explanations: Maybe poorer kids having inadequate access to high-quality health care means they get diagnosed less, or maybe poorer parents are less attentive, or less educated about psychiatric matters. Rich parents are single-mindedly invested in their children’s success, while over-involved upper-class moms and dads need to label every hormonal swing with a new disorder. These pop-psychological explanations make sense, but they’re not true — they describe an imagined set of facts.
A measurable class gap has emerged among children when it comes to mental health.
Here’s the data: The National Health Interview Survey from 2011–12 found that children between the ages of six and 17 from families under the poverty line were significantly more likely to be prescribed psychiatric medication than any other economic group. The same study found that children on Medicaid were 50 percent more likely to get a prescription than those with private insurance. An analysis of attention-deficit/hyperactivity disorder (ADHD) diagnoses among kids between the ages of five and 17 between 1998 and 2009 found rates rose twice as fast for working-class and poor kids. A measurable class gap has emerged among children when it comes to mental health.
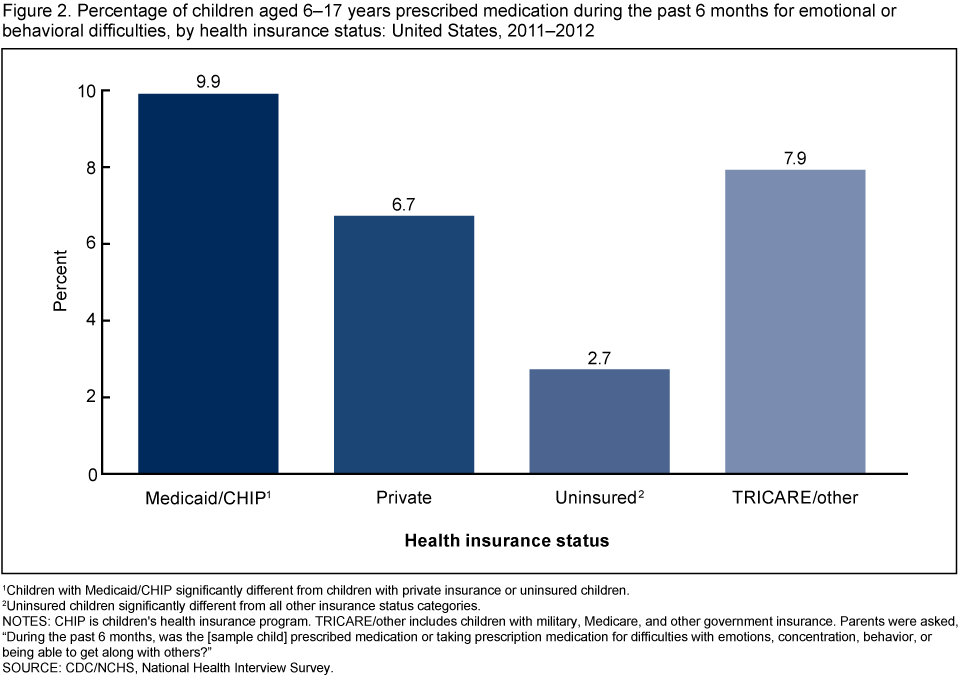
(Chart: U.S. Centers for Disease Control and Prevention)
The idea that mental health is a bourgeois concern, that rich people get depressed while the poor get sad, isn’t just archaic — it gets the statistics backwards. Worse than just being wrong, this idea pollutes the way we think about children’s mental health across the class spectrum.
Ara Francis, a sociologist at the College of the Holy Cross who has studied the ways middle-class families cope with major problems in their children’s lives for her book Family Trouble, told me about her own preconceptions. “I entered into the research with assumptions,” Francis says. “I imagined these intense over-parenting mothers that were labeling kids almost for their own benefit rather than for the children. I had that image in mind, which has become dominant in popular culture, and I was just so surprised that I seemed to find so many grief-stricken families.”
The families Francis talked to had the resources to pay for treatment and medication, but they never set out to produce super-children or to cheat the system. Like most parents, they just wanted their kids to be happy, now and in the future. “The trick becomes that happiness among the middle class in the United States has gotten really bound up with material success and prestigious occupations,” Francis says. “The place where parents started was that to have a happy life means to be successful. And so it was hard for them to imagine a world where a kid would not get a prestigious education and still be happy.” Without a normalizing boost, these parents see their children’s futures slipping away. Of course, it’s not normal to receive a prestigious education — that’s why it’s prestigious — and even less normal if you come from the middle class. By those exacting standards, not many kids are going to be happy.
For middle-class and poor kids alike, a competitive edge is no replacement for a safety net.
What makes the intense mother stereotype that Francis mentioned contemptible — in addition to an always-lurking contempt for mothers in general — is that they’re running up the score. Their kids already have a good chance at success and happiness, but these parents want to eliminate all risk, and aren’t shy about using their money to try and do it. In a zero-sum competitive economy, their gain is likely a poorer child’s loss. The intense mom is shamelessly putting her thumb on an already rigged scale; she’s hogging the happiness. And though some version of this straw-mom probably exists wherever wealth is concentrated, most of them are just moms. The helicopter-parent ethos is rare — few parents have the time and resources necessary — yet it has come to stand for all moms parenting medicated children.
Michael Anderson, a pediatrician in Georgia, used the same unbalanced scale metaphor when speaking with New York Times reporter Alan Schwarz in 2012. Anderson diagnoses ADHD and prescribes stimulants to working-class and poor kids who are struggling in school, and he does it out of a sense of fairness. The doctor doesn’t really believe in the condition per se, he confessed to Schwarz, but his prescriptions still work, Medicaid still pays for them, and the pills still help kids focus in class. “We’ve decided as a society that it’s too expensive to modify the kid’s environment,” Anderson said. “So we have to modify the kid.” With poor and working-class Americans set up to fail in school and on the labor market, the best he can offer is a chemical assist. But just because it’s what he has to offer doesn’t mean it’s good enough.
As part of the NHIS, researchers asked parents of kids on medication for emotional or behavioral difficulties if they perceived a benefit, if the pills seemed to be working. Most parents above the poverty level reported that they saw a lot of benefit (59.2 percent), and only 16.5 percent said not at all or a little. For families in poverty, however, only 43 percent saw a lot of benefit, while 25.8 percent saw little or none. The pills don’t seem to be as effective when they’re used to treat socio-environmental problems.
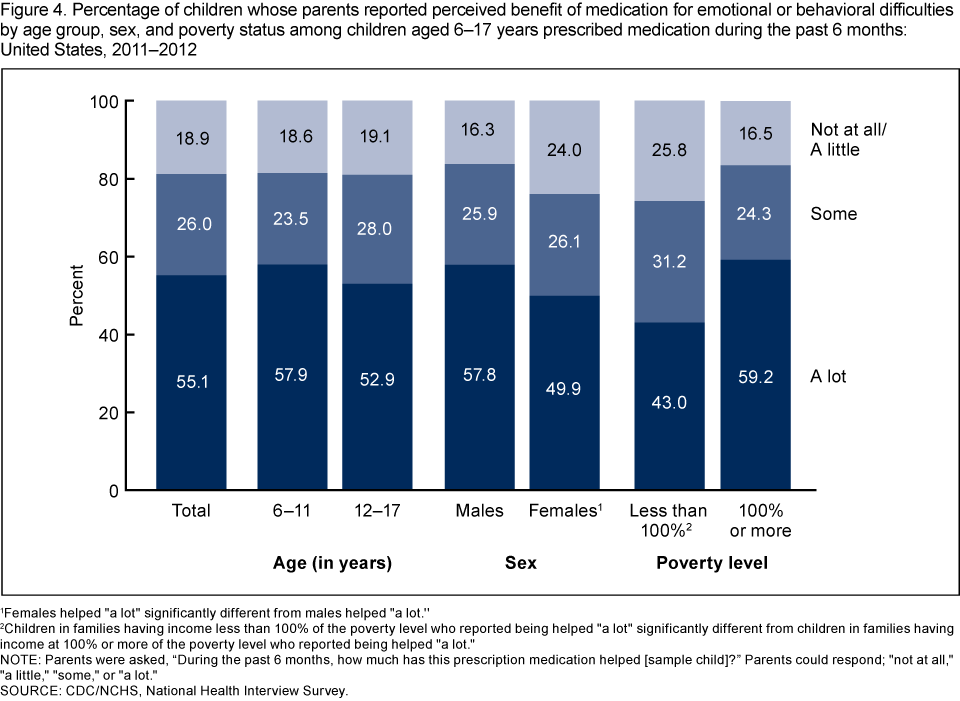
(Chart: Centers for Disease Control and Prevention)F
“Let’s say a kid shows up to school and he’s sleeping in class because the night before there were gunshots outside his house,” says Victor Rios, a sociologist at the University of California-Santa Barbara and a scholar of the lives of black and Latino boys in urban communities. “There’s no condition, he just very simply needs a safe place to sleep. But when he falls asleep in class, that’s diagnosable, that’s attention deficit.” Rios sees a split in mental-health care in the populations he studies: Either the treatment is inconsistent and halfhearted, or it’s extreme and disciplinary. “Kids become clinical cases, when in reality they need to sit down and talk and figure out a solution to a temporary problem,” he says. Treating the child doesn’t work when the child isn’t the issue.
When you consider all the work, knowledge, and infrastructure necessary to supply a kid with Adderall, compared to how little it takes to provide shelter, it’s mind-blowing that American society is readier to provide the former than the latter. But of course, the marginal cost of a quick doctor visit and a supply of pills is smaller than that of social workers and public housing. Between 1994 and 2001, the rate of psychotropic prescription for adolescents between the ages of 14 and 18 increased 10 times as fast as overall psychiatric visits for the demographic. Who needs problems when you have solutions?
There is a whole range of experiences when it comes to children and mental-health problems, very little of it represented in the archetype of the rich mom, her imaginary manicured finger on the scale. Instead we see middle-class kids struggling to keep up, and poor kids struggling to get by. When the exceptional story becomes the one we’re used to hearing, we begin to think of depressed or anxious kids as not really needing help. That’s a problem that demographic data won’t solve by itself, but it can point us to where preconceptions are misconceptions. The qualitative research pursued by scholars like Rios and Francis is vital to understanding what’s actually going on.
“It’s important for us to remember the power of human resilience,” Rios says. “You have children growing up in poverty that face dire conditions, but if we were to provide them minimal but consistent resources, we would get a long way in terms of outcomes. We find that they’re able to figure out ways to heal.” Among the minimal but consistent resources all children — all people — deserve are security and the reasonable expectation of future security. But whether for middle-class families who feel the need to give their kids, as Francis puts it, “every advantage,” or the working-class and poor kids whom Anderson tries to give some advantage, a competitive edge is no replacement for a safety net. This country has abdicated the social responsibility to provide a secure and dependable environment for every child in favor of an individual (and maternal) responsibility to maintain mental balance and academic performance. It’s not working, and we can see why.

||





