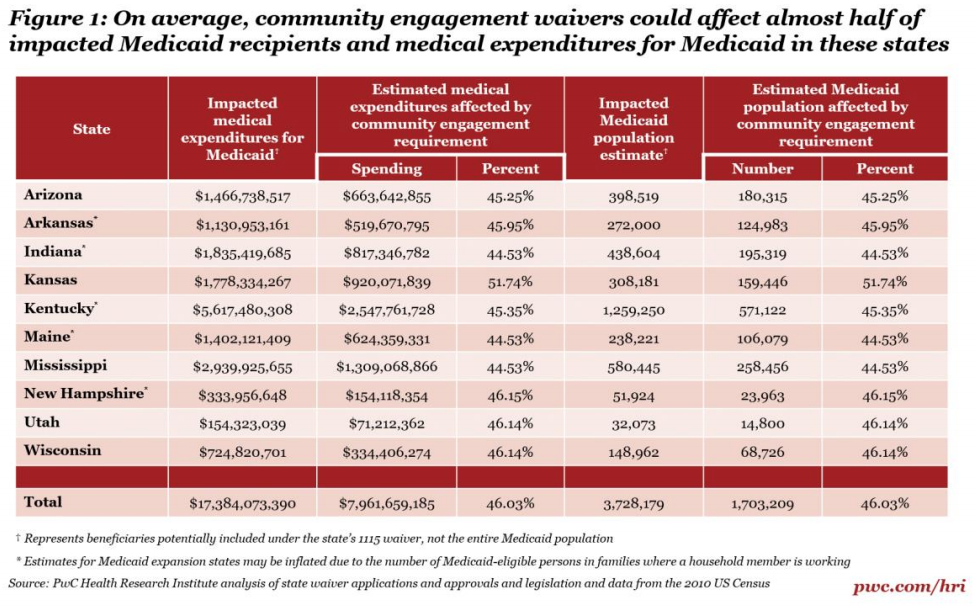
Waivers mandating work requirements for Medicaid beneficiaries could affect approximately 1.7 million people in 10 states, according to an analysis by PricewaterhouseCoopers’ Health Research Institute.
So far, three states—Kentucky, Indiana, and Arkansas—have received approval from the Centers for Medicare and Medicaid Services for their community engagement waivers. Seven other states have applied.
Ten states, listed in the chart below, are seeking to introduce Section 1115 Waivers, which require that Medicaid beneficiaries “maintain or seek regular employment, enroll in an educational program or perform community service” in order to continue to receive benefits.
These waivers could lead to reductions in those insured by Medicaid, and health-care providers in these states could see a steady increase in uninsured patients if they lose coverage due to their inability to meet the new work requirements.
Courts have, in the past, ruled that the work requirements were “impermissible” since states could not adequately explain how these requirements would benefit Medicaid.
Exemptions to these requirements vary from state to state—Medicaid beneficiaries in substance abuse treatment programs would be exempt in Kansas, Maine, Mississippi, Virginia, and Wisconsin. In Kansas, Mississippi, and New Hampshire, beneficiaries undergoing treatment for chronic illnesses would be exempt, and in Arizona foster youth up to age 26 and victims of domestic violence would be exempt.
Despite some exemptions from the waivers, the new requirements would increase the likelihood of consumers moving in and out of Medicaid programs as eligibility changes, according to HRI’s analysis. This would, in turn, put strain on physicians and Medicaid beneficiaries as they try to navigate a new system.





