Something I have a hard time thinking about and quantifying is how many times I will menstruate in my life. Not difficult in that addition is difficult, but difficult in that every time I think about how many times an egg is going to descend down one of my fallopian tubes, I grow exhausted from the sheer frequency.
I got my first period when I was in eighth grade. I was late among most of the girls I knew. I would go on to have irregular and painful periods all throughout high school. When I started birth control around 18, they at least became predictable, but I was still in pain. I was told that’s just what happened. I never asked, or thought to ask, why the four years of pain was so severe.
In a new memoir, Ask Me About My Uterus: A Quest to Make Doctors Believe in Women’s Pain, journalist and advocate Abby Norman uproots the paradigm that women must suffer their pain alone and in silence. She melds memoir and reporting to chronicle how her endometriosis diagnosis unfolded alongside the medical disbelief around her chronic, debilitating pain.
In addition to Norman’s book, recently there’s been Doing Harm: The Truth About How Bad Medicine and Lazy Science Leave Women Dismissed, Misdiagnosed, and Sick, from Maya Dusenbery; Invisible: How Young Women With Serious Health Issues Navigate Work, Relationships, and the Pressure to Seem Just Fine, by Michele Lent Hirsch; and Porochista Khakpour’s upcoming memoir, Sick. All are part of a growing movement of women writing about physical pain and demanding their stories, reporting, and research be heard in the face of medical disbelief.
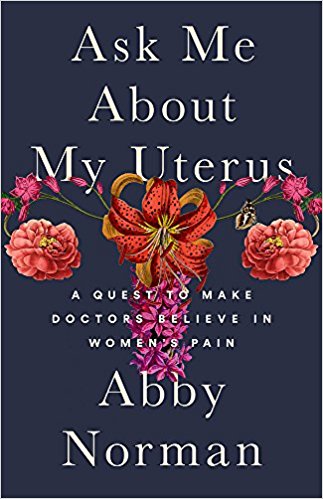
(Photo: Nation Books)
Norman began writing about endometriosis and chronic pain as a way to understand her own condition—endometriosis and chronic pain. She found power through knowledge; she even got a job within a hospital that gave her access to medical literature to further her own studies. But, as she writes, knowledge of her condition was sparse.
Even when she found information about endo (a shortened name for her diagnosis) or learned how to quantify her pain using the same language as her doctors, it didn’t matter. She was able hold down a job; she appeared to be fine, at least on the outside. How could she be in pain? As Norman writes: “I was slowly figuring out that not only was my pain going to be disbelieved, but it was never going to take precedent.”
While Ask Me About My Uterus is a respectable entry into this genre of women’s pain, it also touches on a troubling phenomenon within medicine: the loyalty to fertility above all. The medical devotion to birth and motherhood that only starts in the uterus is hurting everyone. When Norman had her first surgery to drain “chocolate cysts”—cysts filled with old, brown blood—she assumed the doctor hadn’t just removed the cyst but also the ovary, maybe the fallopian tube. After all, the doctor had told her the cyst had displaced her ovary and twisted the fallopian tube behind her uterus.
But only after the procedure did she learn that the doctor hadn’t removed anything—just drained the cyst. The reasoning: doing so would negatively affect Norman’s fertility. Norman had never expressed any severe allegiance to her reproductive ability, but the doctor, a woman, assumed it was important. As a result, Norman realized she needed to clearly communicate that “subfertility” would not be a problem.
“I can only assume that doctors don’t feel comfortable taking a woman’s word for it when she says she’s not concerned about her fertility,” Norman concludes. These are the most powerful passages in Norman’s book, those that question the value we place on fertility at the expense of comfort and health.
As Norman puts it, the patriarchy of pain doesn’t have to be the norm.
“I began to realize that while there are some overarching patriarchal themes, they aren’t solely perpetuated by men,” she writes. “Women do it too: every time a mother tells her daughter that bad cramps are just a part of life, or just a part of being a woman, she’s reinforcing something she’s come to understand as fact.”
But as a young woman advocating for her own body, Norman’s greatest asset (deep knowledge of her own condition) becomes the biggest liability. Norman becomes increasingly concerned with how her gender and sexual expression have affected her treatment at the hands of doctors. To wit, she’s forced to bring her then-boyfriend to a doctor’s appointment so he can confirm that their sex life is interrupted by Norman’s pain:
If I, or any other woman whose gynecologic cancers or pathologies had gone undiagnosed, had just been sick in some other part of the body, in some other way, would it have been any different? Or would it not have mattered? Was the underlying pre-existing condition being female? Does the congenital lack of a Y chromosome predispose a patient to worse outcomes regardless of what condition or disease they present with?
Norman expresses at the start her hope the “this book will no longer be applicable by the time it’s in your hands.” That’s sadly not the case.
In her years-long journey to write the book—which I’ve watched her tweet about for a bit—Norman hasn’t found a solution to her pain. Instead she built a new life within these limitations.




