Stephanie comes into the room spitting mad. After 25 years of injecting crushed-up painkiller pills and heroin—25 years of stealing from her parents, two DUIs, possession charges, selling drugs, all of that—she is 92 days sober. She has just graduated from her 90-day residential rehab, which she says was life-changing. In fact, she liked it so much, she wanted to stay on as what’s called a senior resident, which involves doing small chores and checking that other residents are following the rules that she credits with having helped in her own recovery: getting up early, keeping their rooms clean, and attending classes that taught them about the principles of Alcoholics and Narcotics Anonymous. (Stephanie is a pseudonym; she requested anonymity for this story, to protect her living situation.)
She found it so fulfilling to help other people with addictions that she wants to keep doing so. But, in so many words, her counselor has told her that, to become a senior resident, she’d have to quit her methadone program.
“I was, like, Fuck off,” she says, flipping the bird to an imaginary person to the right of me. “I’m not getting off methadone. It’s the only thing that’s helped me stay clean. I mean yeah, going to the meetings and stuff, but the basis is methadone. It’s the only thing that fills that gap when I was waiting for something throughout the day, and nothing ever came because I wasn’t using. With methadone, I don’t have to use.”
“My life, that hole, is filled,” she says.
We are sitting, just the two of us, in a group therapy room at C.O.R.E. (Comprehensive Opiate Recovery Experience) Medical Clinic in midtown Sacramento, California. Just a few steps out the door are the open windows where C.O.R.E.’s patients get their tiny paper cups of methadone, an opioid medication that’s used to manage addictions to opioid painkillers and heroin. Methadone attaches to the same receptors in the brain to which heroin and pills like OxyContin and Vicodin attach, and can trip the same cascade of brain reactions that produces the warm pleasure that hooks folks in the first place. C.O.R.E. locks its dumpsters, so people won’t go through the trash, looking for dregs.
But unlike pills and heroin, methadone lingers for a long time in the body, helping to alleviate cravings and compulsive drug-seeking—the need to fill the hole. At the right dose, it doesn’t produce a high; it’s meant to give people the brain space they need to stabilize their lives and focus on therapy. A regimen of therapy plus methadone—or one of two other Food and Drug Administration-approved medications, buprenorphine and naltrexone—is considered the gold standard for opioid addiction treatment. Studies show that, compared to getting no medicines, methadone and buprenorphine keep people in treatment for longer and reduce how much they cheat with illicit opioids. The medicines also save lives: Compared to getting no treatment, methadone can cut death rates by 75 percent.
An estimated 47,600 Americans died of an overdose involving opioids in 2017, a larger population than that of most towns in the United States. Opioid-involved overdoses are America’s top cause of accidental deaths, outstripping car crashes. The country’s overdose problem is so severe, it’s contributed to a slight decline in life expectancy for three years in a row now. Stephanie’s home state of California actually has a lower overdose rate than the national average, but rates are still high in certain counties, especially in the state’s rural north, and officials are worried.
In response, the government at both the state and national levels has mustered resources to try to make what’s known in the industry as “medication-assisted treatment” (MAT) available to everyone who needs it. MAT and the science behind it have been around for generations now, but never has there been such a united push to promote it because there’s never been an overdose epidemic like this.
Yet at recovery centers in California that say they treat people with opioid addictions, MAT is often not available on site. Some centers are resistant even to letting their participants get MAT elsewhere.
“My counselor told me three separate times: ‘I’m not asking you to get off methadone, but…‘” Stephanie says.
The counselor never explicitly said the program didn’t want a senior resident to be on methadone, but she gave Stephanie the impression that it was only some “legal thing” that kept her from saying so. A woman who picked up the phone, when I called the headquarters of Stephanie’s program, confirmed it’s possible for a site supervisor to make such a rule about senior residents, but she didn’t know whether such a policy was in place at the moment. She declined to give me the number for the women’s residential site supervisor.
There’s no law that says treatment centers can’t make being MAT-free a condition for holding special positions within the center, but new regulations do push for basic MAT acceptance. Any center that’s opted into a new program for which the state pays the costs of expanded addiction services for low-income patients on Medi-Cal, California’s version of Medicaid, must accept MAT patients. In January, a state law went into effect that requires all residential addiction treatment facilities—which must be licensed by the state—to take clients who use MAT, even if the facility doesn’t get any government money at all.
“So [my counselor is] like, ‘We want you to decide on your own,'” Stephanie says. She chose to stay on methadone. She’s now living in a transitional home—a step down in addiction treatment, like moving from critical care to a regular hospital room. Her home is run by the same organization that runs her residential rehab, and, for now, she’s deferring her plan to become an addiction counselor. As a next step in her recovery, she’s looking for another job.
‘Without Ongoing Recovery Maintenance, Detox Sets People Up to Overdose’
To learn about how many addiction treatment programs don’t use MAT and why, I’ve spent the past few months analyzing publicly available data from California and federal agencies. Although the policies and exact numbers I found are specific to the Golden State, they’re a window into a process that’s happening nationwide, as the federal government planned to give up to $1.2 billion to states over five years to expand access to MAT and help end the opioid crisis.
What I found is that, despite the government’s efforts, some parts of California still lack basic facilities for MAT. Eight of the top nine California counties with the highest opioid overdose rates in 2017 don’t have a single methadone clinic.
In addition, I identified almost 100 California facilities that confirmed for me over the phone that they treat opioid addiction, but don’t offer MAT. Another several hundred facilities aren’t licensed to provide MAT. That doesn’t mean clients at those facilities can’t get MAT. Like Stephanie, they could get medicine in one clinic and additional counseling somewhere else. But such a bifurcated system forces already vulnerable people to get treatment in two different places that may send them conflicting messages. State and county officials are trying to get everyone on the same page, but some treatment providers I talked with thought it would take years to do so. What happens to those who come into the system in the meantime? “We’re hoping it’s not going to be a bad experience,” says Garrett Stenson, C.O.R.E.’s program director.
Finally, a significant minority of treatment centers are reluctant to embrace MAT for philosophical reasons. There’s a lingering belief among some in the treatment industry that taking methadone or buprenorphine is trading one addiction for another. “Oh, no, no, no, that’s not recovery,” the man who picked up the phone at Latinos Recovery Home in Los Angeles told me in November. “That’s just a Band-Aid from one drug to another.” (Nobody at Latinos Recovery Home responded to a request for comment in April, after the law requiring licensed residential centers to accept MAT patients had gone into effect.)
It’s true that methadone and bupe are both opioids, can produce highs, and can make people overdose. People can resell these medications on the black market, just as they do prescription painkillers like OxyContin and Percocet. A third FDA-approved MAT medication, naltrexone, works a bit differently from the other two: It hugs the opioid receptors in the brain tightly, preventing addictive opioids from slipping in and triggering euphoria, so it’s not as controversial. But one study found that only about 11 percent of people stick to their naltrexone treatment. Addiction doctors like to see clinics have all three medicines on deck, so patients can use the one that works best with their brain chemistry.
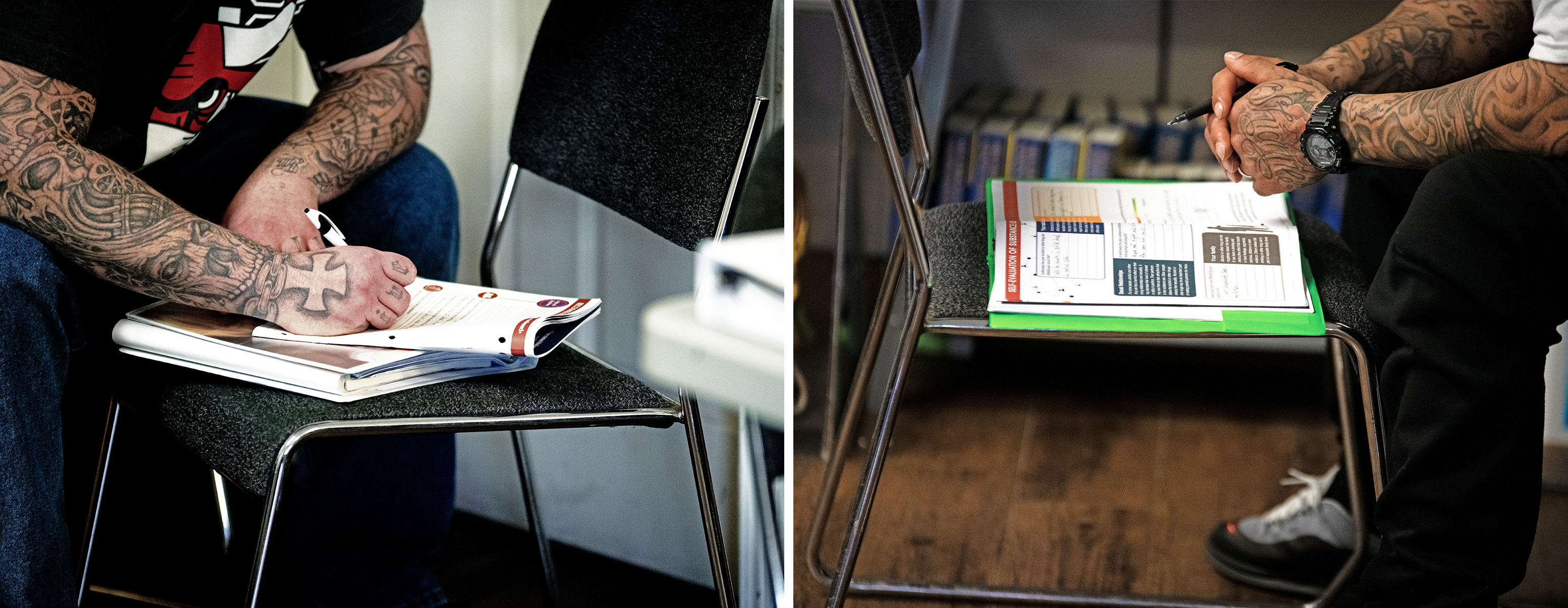
(Photo: Salgu Wissmath)
Beyond that, the alternatives are grim. The irony of seeking any help for opioid addiction is that, while it’s the first step toward reclaiming a life, it also puts people in a precarious position. The brain gets used to being flooded repeatedly with opioids, whether from pills, heroin, or other street drugs. As the body builds tolerance, it starts reacting less, which means that users get less of a high: Nothing’s like the first time. A less-reactive brain also means opioids don’t trigger side effects, like suppressed breathing, as strongly in heavy users.
Once someone has undergone a detox, however, her brain’s sensitivity to opioids rebounds. If she falls off the wagon and tries to take a hit of a similar size to what she would have used before treatment, it can overwhelm her brain and stop her breathing.
Several years ago, Kodi Gimblin, another C.O.R.E. client, picked up one of her friends from rehab and drove him—as he requested—to his heroin dealer. “I was one of the few that he knew would show up for him,” she tells me via text.
Before she dropped out of college, Gimblin was taking classes to become a nurse, so she knew what would happen. Her friend wasn’t on methadone because his insurance didn’t cover it, she says. She begged him not to inject as much as he’d used to. Even his dealer tried to explain.
“He kept telling me that he hadn’t even been clean for two months, it’ll be fine,” she writes. “[H]e didn’t even get the whole shot inside his arm when he overdosed.” She drove him to the emergency room, and he survived the overdose.
“That’s the tragedy of detox,” says Brian Hurley, an assistant professor of addiction medicine at the University of California–Los Angeles. “Detox sets people up to overdose unless people are participating in some ongoing relapse prevention or recovery maintenance”—that is, ongoing dosing with methadone, buprenorphine, or naltrexone.
Most people stay on MAT for anywhere from six months to three years. Relapses are common among those who stop before two years. For those with deeply entrenched addictions, it’s possible to be on MAT for life. America may just be waking up to its opioid addiction crisis now, but for those affected, it will take years—maybe a lifetime—to heal.
When the Doctor Tells You to Keep Using Heroin
The part of California that’s been hit hardest by opioid overdoses sits outside the popular conception of the Golden State, which is bracketed by San Francisco in the north and Los Angeles in the south. Californians call the San Francisco Bay region Northern California, or “NorCal,” but, geographically speaking, it’s more like MidCal. If you were taking a road trip up the state, you’d still have five more hours of driving from SF before you hit the Oregon border.
Gimblin is from northern-northern California, which is a patchwork of farmland and forest. She grew up in Princeton, a 300-person town whose downtown comprises six blocks on the west bank of the Sacramento River. You can see the stars out there, and she swears you can breathe better. When she was a kid, the family had a lot of parties, had people over for drinks and card games. “I was a textbook alcoholic, but a functioning one,” she says. That wasn’t so long ago. Gimblin is only 26. She started smoking Opana, a prescription painkiller, and injecting heroin, during college.
Green-treed, true northern California is severely lacking in MAT options. The nine counties in California with the highest overdose death rates in 2017—the latest numbers available—are all in the state’s far north. Eight of them, which together are home to more than half a million Californians, don’t have a single methadone clinic, according to the state’s latest records.
The good news is that these places do have higher-than-average numbers of prescriptions for buprenorphine, a MAT option that works, in low doses, much like methadone does. At high doses, buprenorphine blocks opioid receptors in the brain, which reduces the risk of overdose. Unlike methadone, which has to be dispensed in federally licensed clinics, any doctor who undergoes training can prescribe buprenorphine. So even in a county like Humboldt—America’s weed-growing capital, whose center is 152 miles away, by car, from the closest in-state methadone clinic—residents can still get a buprenorphine prescription.

(Photo: Salgu Wissmath)
The availability of bupe in rural northern California is relatively new, helped by a nearly $45 million grant the state received in 2017 from the federal government. Using the money, the state launched a project aimed at California Native American tribes, plus something called Hub and Spoke, which is designed to link remoter clinics to central “hubs” that have more experience and training in addiction treatment. In Hub and Spoke’s first year, more than 7,000 Californians started MAT treatment, or about 18 percent more than started in the period immediately before the grant took effect.
Gimblin remembers what it was like in northern California before Hub and Spoke was a twinkle in anybody’s eye. After high school, she went to college in Chico, a city of about 90,000 that’s 30 miles away from Princeton, situated between the Mendocino and Plumas National Forests. “I was out living on my own, thought I knew everything,” she says. She waitressed, partied, and started dating a guy she’d gone to school with, who introduced her to pill-smoking.
In 2012, she discovered she was pregnant and went to a doctor, who told her she should get on methadone, which would help stabilize her addiction while continuing to provide opioids to her and her baby. Withdrawing suddenly from drugs at that point threatened to put the fetus into distress, or even to trigger a miscarriage. Buprenorphine is also a good option for pregnant women to stave off withdrawal, but apparently the doctor didn’t know of any nearby prescribers.
The nearest methadone clinic was in Sacramento, the state capital, almost 90 miles away. Chico wouldn’t get its first methadone clinic until 2014.
Gimblin told her doctor she couldn’t get to Sacramento at that time. So, in the meanwhile, she says: “He told me to keep using.”
She and I are talking in the same group therapy room at C.O.R.E. where Stephanie and I met. Gimblin has a long, blond braid, pulled back perfectly smooth from her temples, like an athlete’s. She plays with the end of it sometimes, when she talks about uncomfortable topics.
She ended up losing the baby. Her boyfriend at the time had become abusive. One night, he demanded the car key and her tip money. When she resisted, he beat her, and she miscarried. It took a lot of therapy for her to learn not to feel guilty about that, to understand that it wasn’t her fault just because she wouldn’t give up the key.
One thing that sticks in her mind is the doctor emphasizing how important it was that she not quit heroin cold turkey.
“He was telling my boyfriend at the time: ‘You need to make sure that she has something every morning and every night,'” she says. “Damned if you do, damned if you don’t.”
Getting Past ‘Abstinence Only’
What about the regions where treatment centers exist, but don’t offer MAT? To learn more about these, in November and December, a fellow reporter and I called all the facilities in California that had indicated that they don’t offer MAT on a voluntary survey they sent to the federal government’s Substance Abuse and Mental Health Services Administration. I talked to whoever picked up the phone at the number listed with SAMHSA. Typically, I spent just a few minutes with each facility, asking if they offer MAT and, if not, why.
Staff at 97 facilities confirmed that they treat people for opioid addictions, but don’t offer MAT on-site. Of those, 30 said they were philosophically opposed to MAT. Very few told me that they had trouble with resources.
“Why don’t you offer MAT on-site? Is there a shortage of doctors there who are licensed to prescribe it?” I asked the Lucerne Community Clinic in the northern county of Lake. Lake has California’s fourth-highest rate of deadly overdoses, and more than one in five residents lives in poverty. I was trying to sound sympathetic.
“Actually, it’s just the opposite,” the woman on the other end of the line replied. There were plenty of doctors around who were able to prescribe buprenorphine, she said. Since the clinic is not licensed to dispense medications, Lucerne referred clients out as needed.
In America’s most populous state, having a few shy of 100 opioid-treatment facilities that don’t offer MAT might not sound so bad. But the problem could be much more widespread.
Many treatment centers don’t send their stats to SAMHSA. For example, California’s Department of Health Care Services lists 1,889 licensed residential facilities and certified alcohol and drug programs. SAMHSA, meanwhile, only has information on 1,183 “substance abuse” facilities for the entire state.
California has among the highest proportion of facilities that say they treat opioid addiction without MAT, according to the SAMHSA data I analyzed. About 15 percent of SAMHSA-listed, opioid addiction-treating California facilities say they don’t offer MAT. The national average is 12 percent, and, in nine states, that number is less than 5 percent.
In addition, while we don’t have a SAMHSA checkbox asking whether these centers offer MAT, we do have some other, suggestive information about the hundreds of California addiction treatment facilities that aren’t listed in SAMHSA. The state Department of Health Care Services records whether facilities in California are licensed to provide “incidental medical services.” Facilities that aren’t licensed for incidental medical services can’t prescribe or dispense MAT medications, although if a resident comes to them with take-home doses, the facility can store those in a locked safe.
Based on listings I downloaded in October of 2018, I found several hundred addiction treatment facilities that are licensed or certified by the Department of Health Care Services, don’t appear in SAMHSA’s database, and aren’t licensed for incidental medical services. In my SAMHSA calls, I talked to dozens of facilities that don’t offer incidental medical services. Their approaches to MAT varied widely.
Some, like the Lucerne Community Clinic, referred their clients to nearby buprenorphine prescribers or methadone clinics. Addiction specialists generally don’t consider that to be an ideal arrangement.
“A patient-centered approach would be to put this all in one place,” says Sharon Levy, director of the Adolescent Substance Use & Addiction Program at Boston Children’s Hospital.
If the split system is all that’s available, however, at least patients are still learning about and receiving all the components of the recommended treatment. “If patients are happy with it, who am I to say that’s wrong?” Levy says.
Other facilities seemed to leave it up to their clients to discover and obtain MAT on their own. The woman who picked up the phone at River City Recovery Center’s facility in Herald, California, said that if someone came in and was already in a methadone program, River City would accept them. A program director told Pacific Standard this month that if someone came asking about MAT, staff would tell them about local providers. But the staff doesn’t systematically refer people to such services.
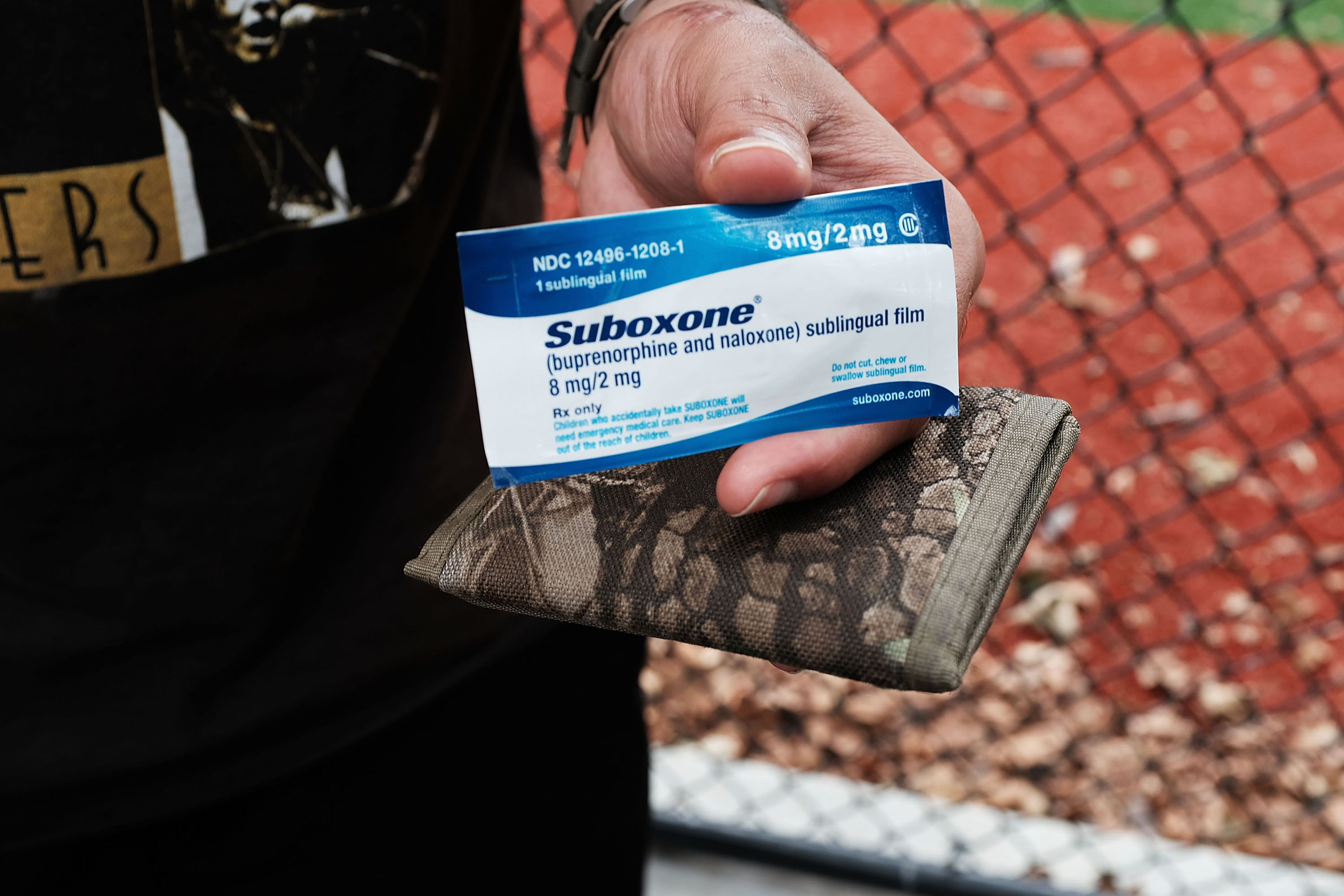
Finally, of course, there are those centers that oppose MAT altogether. “That’s not our policy, to trade addiction for something else.” (Native Directions, Inc.’s Three Rivers Lodge in San Joaquin County.) “We don’t even allow any of our clients to be on ‘Suboxygen,’ methadone, or whatever.” (Father Alfred Center in San Francisco; one brand name for buprenorphine is “Suboxone.”) “This is a 100 percent Christian, faith-based organization. They quit cold turkey. It’s taking that leap of faith.” (Inland Empire Teen Challenge in Riverside, California. Although some teens won’t need MAT because they’re newer to opioid abuse, it’s still crucial and lifesaving for many, Levy says.)
To clarify, I would ask these places: “Does that mean it’s your policy that people in your program can’t be on methadone or Suboxone?” or “So you’re philosophically opposed to methadone and buprenorphine?” They all confirmed.
In September of 2018, the California state legislature unanimously passed a law that says licensed addiction treatment centers can’t refuse clients just because they’re on MAT. I made my calls in November and December. The law went into effect in January. In April, Pacific Standard tried to contact the facilities named here again by email. Ramona Valadez, the Three Rivers Lodge’s executive director, wrote only: “Our policy had changed. We are working with MAT.” The senior program manager of Father Alfred Center said staff are working on complying with the law. Inland Empire Teen Challenge’s director noted the program is not licensed by the state, so does not need to comply with the law.
A few of the facilities I talked with were aware of the law and had historically been “abstinence-only.” These programs were open about how hard it is to change tack. For the man who picked up the phone at the Chabad Residential and Outpatient Treatment Center in Los Angeles in December, the new law represented a clear affront to what Chabad teaches its clients. “We’re saying to people, ‘We want you to be clean and sober, and that’s the starting basis for your recovery'”—and yet now, in the center’s eyes, Chabad must accept clients who aren’t clean. In April, Donna Miller, the center’s clinical director, wrote that Chabad’s policy had actually changed over “the last few years,” although she said it’s still a “challenge” to ensure clients are on the right dose of MAT medications “to help maintain their over[all] goal of sobriety.”
Changing Philosophy to Stay in Business
The treatment centers of Yolo County, California, know what it’s like to launch an MAT program in a place with a long history of abstinence-only orthodoxy.
The day I drove into Yolo, in mid-March, the almond crop was in full bloom. The tops of the closely planted trees interlaced to create long, continuous clouds of fragrant fluff. By the end of the week, half of those silky petals would be on the ground, and bright green leaflets would appear among the flowers.
Yolo is located along the gateway between the Bay Area and California’s far north, about an hour and a half north of San Francisco. It has a population of around 220,000 and an opioid overdose rate roughly around the state average. Yet there has never been a methadone clinic here. One hundred and sixty Yolo County residents travel to Sacramento or farther, many of them likely daily, to get methadone, says Ian Evans, Yolo’s alcohol and drug administrator.
(Photo: Spencer Platt/Getty Images)
C.O.R.E. has been trying to build a facility in Yolo for 15 years but has always run into community resistance, says Marshall Stenson, C.O.R.E.’s business services director and Garrett’s brother. In 2015, there was talk of opening a facility in Woodland, the bucolic county seat. City council members objected to the clinic’s proposed location near two schools, Woodland’s Daily Democrat reported at the time. Eventually, C.O.R.E. settled on renovating a former trucking school in a semi-industrial part of West Sacramento, a city on the county’s southeastern edge. From the county’s center, it shortens the drive to the nearest methadone clinic by less than 10 minutes. It opens in May.
In the meantime, 55 locals get their MAT at a CommuniCare clinic. In March, I visited one of CommuniCare’s Woodland locations, not too far down the road from a tractor dealership and the Yolo County Farm Bureau. The clinic has separate entrances for its primary care and behavioral health services, but behind the front desks, it’s all one continuous warren of hallways and offices.
CommuniCare clinics have served farm workers and other low-income residents of Yolo since 1972, and they have always treated addiction. It was only in 2016, however, that the clinic’s leaders decided they wanted to offer buprenorphine for opioid dependence. For many years, they’d seen mostly people with addictions to methamphetamine, which isn’t helped by MAT and is still the most widely misused drug in the county. Recently, however, the clinic started getting folks saying they smoked meth and opioids. Many were young. “Kids, really—young adults,” says Sara Gavin, CommuniCare’s chief officer for behavioral health. They also had many chronic pain patients who were on high doses of opioid painkillers, at a time when the federal government was pressuring funded clinics to cut back on prescribing opioids. CommuniCare needed something else to give those patients.
Historically, CommuniCare’s addiction treatment had been abstinence-only. The changeover to MAT was hard, staff say.
“There was some education that had to happen with some of our counselors who have personal experience in recovery and recovered through the 12-Step community,” Gavin says. Many of the programs I’d talked to that were philosophically opposed to MAT were based on Alcoholics and Narcotics Anonymous’ 12 Steps. Those are the ones that begin with admitting that you’re powerless over your addiction and end with having a spiritual awakening as a result of the steps. The 12 Steps emphasize working with others who have walked the same road of addiction, rather than depending on hierarchal doctor-patient relationships. A careful analysis of 12-Step programs for alcoholism found that there are few strong studies about their effectiveness, and they seem no better or worse than other psychosocial treatments.
Still, they really resonate with some, including Stephanie. “It is a great program,” she says. “Working the steps, working with a sponsor, everything.”
One principle of Narcotics Anonymous makes it difficult to square with the best available science, however. Narcotics Anonymous’ ultimate goal is “complete abstinence from all drugs.” Members are supposed to have “a desire to become clean one day,” according to official literature. MAT, on the other hand, is supposed to be open-ended, according to the American Society of Addiction Medicine’s national guidelines. Patients can decide they want to step down from methadone or buprenorphine as they progress, but they’re not supposed to go in with an end date in mind.
“There’s some stigma that continues around people being on medication for a long time,” Gavin says.
When CommuniCare first launched its buprenorphine program in 2016, Gavin had to explain to the staff and community the science behind MAT, and why CommuniCare was starting it. She called a couple of her counselors into her office for serious talks. In March, she and a few of her colleagues caught me up on how the transition went, in that same office.
Other challenges, they said, had included getting CommuniCare’s primary-care doctors on board with prescribing buprenorphine. Primary-care doctors don’t get a lot of training on addiction in medical school, and people with addictions are seen as tough patients: They relapse often. Sometimes they lie. (Though who among us hasn’t fudged to the doctor about what exactly our diet is, or how much we normally drink?)
On both the primary-care and behavioral-health sides, staff found it difficult to have to coordinate with a whole new team of professionals.
“I’ve spent so much time in Sara’s office saying: ‘Sara, I don’t even want to do this anymore,'” says program manager Christina Andrade-Lemus, who has a background in social work. She slides down in her chair in mock frustration.
I ask how long it took for the whole clinic to work out these differences.
“Several months,” Andrade-Lemus says.
“I would say a year,” Gavin says.
“Yeah, several months, several months.”
The result, though, is exactly the ideal that experts are pushing for: a clinic where people with addictions can get their medicine and counseling in the same place, where all of their health-care providers know and talk to each other. And all of that is available to any Yolo County resident, regardless of their ability to pay.
But what if you need something more? What if your addiction is so severe, you need constant supervision and someplace to stay, away from places you’ve used and the people you’ve used with, for months or years? Then you’ll need a residential program—and those, industry insiders say, can often be the most resistant to MAT because of their long association with Narcotics Anonymous.
About two miles away from CommuniCare is Walter’s House, a non-profit residential treatment center for adults, housed in a California mission-style building with pink stucco walls and a tiled roof. There’s a small plaque showing Walter Zeck, the minister who founded the program, just inside the locked front gate. Doug Zeck, Walter’s grandson, is now the program’s executive director.
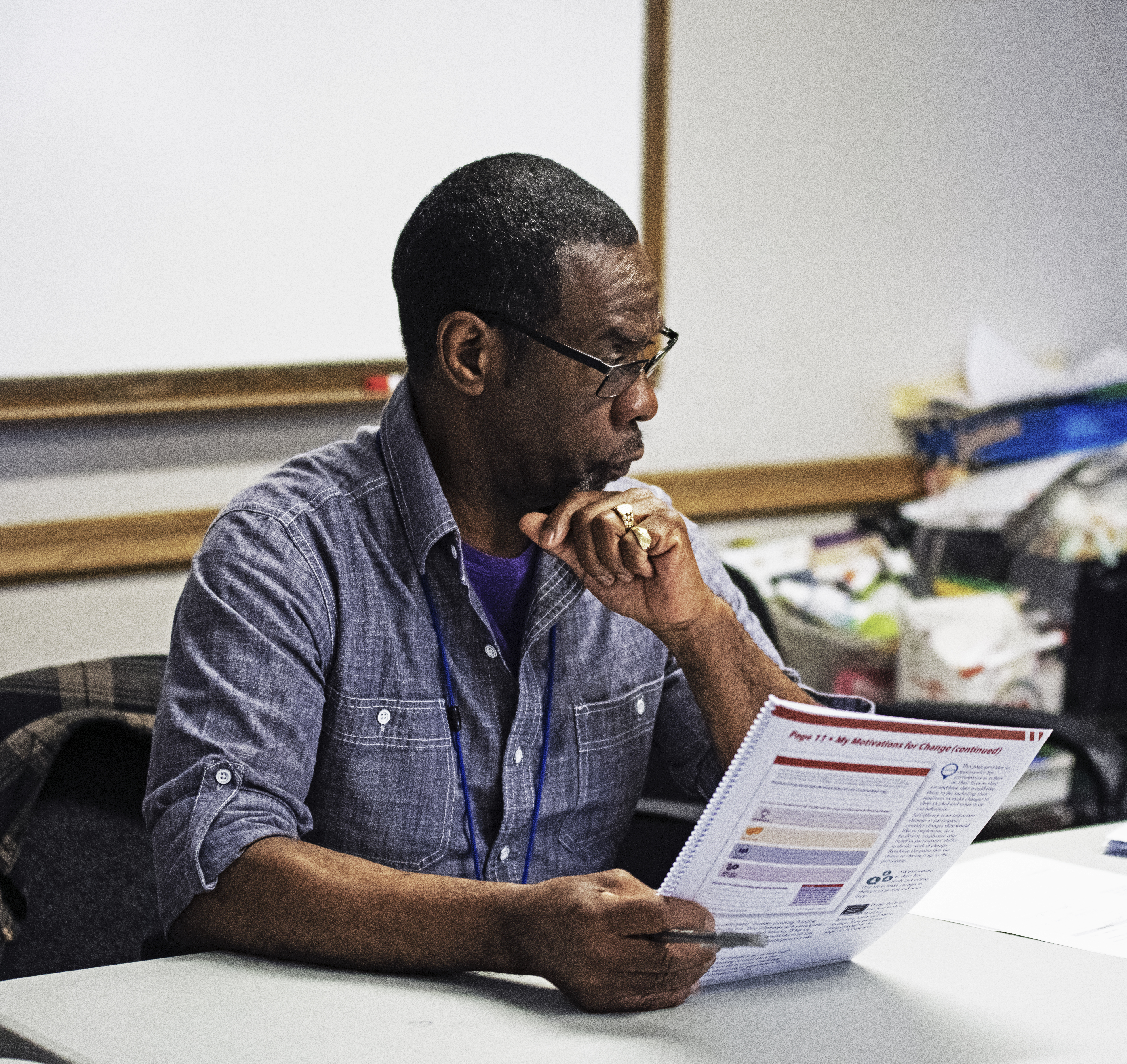
(Photo: Salgu Wissmath)
Until recently, Walter’s House was an abstinence-based, social-model program, which meant that it emphasized peer support and the 12 Steps. “I personally appreciated what we did,” Zeck says. “It wasn’t for lack of success that we embraced this clinical model. It was more out of necessity to have a future.” Walter’s House itself still doesn’t provide MAT, but the program accepted its first client on MAT last fall.
Zeck saw that the treatment industry was moving toward a more medical model of addiction treatment. Yolo County stopped contracting with residential facilities that don’t accept clients on MAT. Zeck also wanted to sign Walter’s House up for the program where the state, through Drug Medi-Cal, would pay for more addiction treatment services. He didn’t want Walter’s House to be too expensive for people who rely on Medi-Cal.
Two of Zeck’s staff quit upon the change. He’s heard of other programs that lost 30 percent of their employees. But he says those who left Walter’s House weren’t necessarily upset about MAT. The new Medi-Cal program required many new practices. When someone broke a house rule, staff couldn’t just kick the client out like they used to. They had to talk through why the client made a mistake. The state effectively implemented this rule because people with addiction who have been kicked out of rehab are extremely vulnerable: They’re still in the throes of addiction, and they’ve detoxed, so they’re liable to overdose.
“I don’t know if turnover or attrition in staff is entirely philosophical,” Zeck says. “Some of it’s just the extreme amount of change, and that’s difficult.”
‘I Don’t Know Who the Hell I Am Sober’
There’s some research that shows MAT medications are effective on their own, without any additional counseling. One major experiment, the Prescription Opioid Addiction Treatment Study, found that study participants who underwent extra counseling that focused heavily on lifestyle change didn’t do any better than volunteers who got only the briefer, medication-focused counseling that primary-care physicians typically offer (which does also talk to patients about lifestyle and encourages them to go to self-help groups).
But those recovering addicts I spoke with at C.O.R.E. in Sacramento, and whom I’ve interviewed over years of covering addiction, often talked about how important therapy was in fighting their addiction. Some have trauma to process. Even without a tough childhood, just spending a lot of time using can expose people to something akin to a quiet, domestic war.
Gimblin has seen five people overdose in front of her and had 10 close friends die. Because she’d taken those nursing classes, she was often the one responsible for bringing people back from the brink. “I’ve had to throw people in a cold shower before, with their clothes on,” she says. (The Harm Reduction Coalition notes that this strategy could work—or it could send the person into shock.) Naloxone, the opioid overdose-reversing drug, wasn’t readily available in Chico when Gimblin was living there. Hospitals likely had it, but she and her friends were reluctant to call 911 and get police involved, especially before California passed its Good Samaritan law in 2013, protecting drug users from prosecution if they sought medical help for an overdose.
Not that Gimblin always used her medical knowledge for good: Friends also turned to her to find good veins in their ruined arms where they could inject.
There’s something that happens when you get on MAT. Suddenly that hole is filled, and you can find yourself with a lot of time, which you used to spend trying to get drugs, taking them, and repeating the cycle.
“I don’t know who the hell I am sober,” Stephanie says, “because I’ve never been sober.” Therapy can help with that.
Gimblin’s been sober longer than Stephanie, about nine months solid, plus two years off-and-on before that. About three years ago, she moved to Sacramento to be with a man she’d met in front of a dope house, who was friends with a couple she knew.
“Yep, not the best of stories,” she says. “But we’re both clean now, so it works.”
Gimblin and her now-fiancé started seeking help when Gimblin found out she was pregnant again—news she was not excited about. “I immediately started crying,” she says. “I knew it was going to be a really hard and long road.” For her, abortion was not an option.
She was still bawling when her fiancé got home from work, and she told him about the pregnancy. “He was really happy,” she says, opening her eyes wide in a what-the-hell expression that makes the photographer and me laugh.
“He was like: ‘Why are you crying? This is amazing!'”
She remembered what her doctor in Chico had told her about staying on a managed opioid regimen, so she called C.O.R.E. and got on methadone. It wasn’t enough to beat her addiction: She kept using while pregnant. Her son, Ryker, was born with neonatal abstinence syndrome—basically baby withdrawal, accompanied by sobbing and shaking that often needs to be treated with morphine. Ryker had to stay in the neonatal intensive care unit for 22 days.
“He wasn’t as bad as some babies I saw in there, but still, knowing that it was your choice and basically your fault,” Gimblin says. “I mean, that sucked.”

(Photo: Salgu Wissmath)
She says Child Protective Services opened a case on her family, which forced her fiancé to enter residential treatment, or else lose parental rights. Gimblin decided to go to rehab also, since, she says, “I obviously needed it too.” They wanted to join a transitional home together, but the only one they got into didn’t accept clients on MAT. They ended up attending separate programs. After leaving the hospital, Ryker lived first with his father’s sister, then with his father’s parents.
After they’d both graduated from residential, Gimblin and her fiancé had to provide frequent clean urine tests, go to counseling, and check in with family court for months, or else face having Ryker legally taken from them. Gimblin relapsed once, near the end of the program, which prompted Child Protective Services to extend its case on them. Then, last August, the agency closed its file on the family. Gimblin says she hasn’t used since.
The three of them now live with Gimblin’s fiancé’s parents, paying $500 a month to rent a house in Sacramento. For now, the dad works, and Gimblin is a stay-at-home mom. She loves her morning routine with Ryker: They wake up, cuddle in bed, and watch a little Word Party. Then they get dressed, have breakfast, and maybe go to the park, or Ryker gets into one of the things he’s interested in right now: drawers, stacks of paper, throwing balls—and the dogs, who, unfortunately, aren’t such fans of him and usually run away. “I feel so bad for him because he’s trying so hard!” Gimblin says.
With her counselor, Gimblin is working on building her relationship with her fiancé and looking, tentatively, for new friends. She’s stable and sober for the first time in almost nine years, but there’s no old life for her to go back to. Nine years ago, she had a fake ID and went out drinking all the time. Just the weekend before I saw her, three of her girlfriends came down from Chico, rented a hotel room in Sacramento, and invited her bar-hopping. But C.O.R.E. has taught her that she shouldn’t drink.
“I need to find some mom friends, I guess,” she says. “I just need someone to understand that they don’t come first. My kid does.”
As for her fiancé, they’re trying to figure out things they can enjoy together other than using drugs. Right now, they can’t quite connect at the end of a hard day the way many couples do.
“If that other person is having a bad day, you guys can easily justify, like, ‘Oh hey, want to go get a sack?'” she says. “That’s been our downfall, unfortunately, is one trying to open up and express that they’re having a bad day and feel like using, and then the other person playing on it. It’s just the evil, yucky addict mind. Like what normal couple would purposefully bring the other one down?”

(Photo: Salgu Wissmath)
Instead, when she has a bad day, she talks with her counselor. C.O.R.E. requires her to meet with a counselor once a week, which she says other clients don’t like, but she appreciates. “I think if people utilized that more, I think it would make sense to them,” she says. “We obviously have some sort of problem going on.”
She worried at first that she wouldn’t like her fiancé without the heroin, but so far it’s working out. He’s good to her, and he’s Ryker’s father. They’re going to move somewhere on their own soon, because the landlord is selling the house where they’ve been living with Ryker’s grandparents. She doesn’t love city living, so she hopes they can move out of Sacramento. She’s thinking of a town 30 miles east, toward the Eldorado National Forest. Out there, they could breathe better, and see the stars. ❖
This story was reported with the support of a 2018 data fellowship from the USC Annenberg School of Journalism’s Center for Health Journalism.

Author: Francie Diep is a staff writer at Pacific Standard, where she specializes in health and drug policy and the intersections of culture and science.
Photographer: Salgu Wissmath is a photographer based in Sacramento, California, whose current work explores the intersections of conceptual documentary and photojournalism, especially as they relate to the intersections of mental health, queer identity, and faith.
Editor: Ted Scheinman
Researcher: Maya Dusenbery
Picture Editor: Ian Hurley
Copy Editor: Leah Angstman
Additional Reporting: Emily Moon




