This week is Mental Illness Awareness Week, a time for advocates to promote treatments for people with mental illness. Mental-health issues affect millions of Americans—about one in five adults in the United States experience mental illness in a given year—but social stigma and dated science still prevent many from seeking treatment.
But new research may aid those advocating for reforms in mental-health treatment and policy; researcher Nev Jones’ work on schizophrenia, for example, shows how early intervention reduces trauma for patients and family members.
Meanwhile, in honor of Mental Illness Awareness Week, here’s a collection of our best reporting on mental illness:

The Touch of Madness
Nev Jones has since made a larger version of this question—of how we think of and treat the mad, and why in the West we usually shunt them aside—her life’s work. Most of this work radiates from a single idea: Culture shapes the experience, expression, and outcome of madness. The idea is not that culture makes one mad. It’s that culture profoundly influences every aspect about how madness develops and expresses itself, from its onset to its full-blown state, from how the afflicted experience it to how others respond to it, whether it destroys you or leaves you whole.
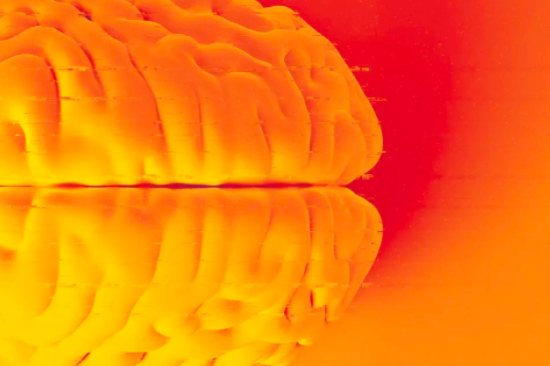
Brain-Altering Science and the Search for a New Normal
The Mass General researchers are convinced that, with this sort of knowledge, they can create an implant that will work for most people with psychiatric illnesses that resist other forms of treatment. The key, they think, will be creating a smart, self-adjusting system—exactly what DARPA called for. Their dream system would have to record brain activity all the time. It would sense when and how a symptom begins to rear its head inside yours. It would zap all the right places at the right times to combat disordered thinking, and in real-time would return your brain to its normal state.
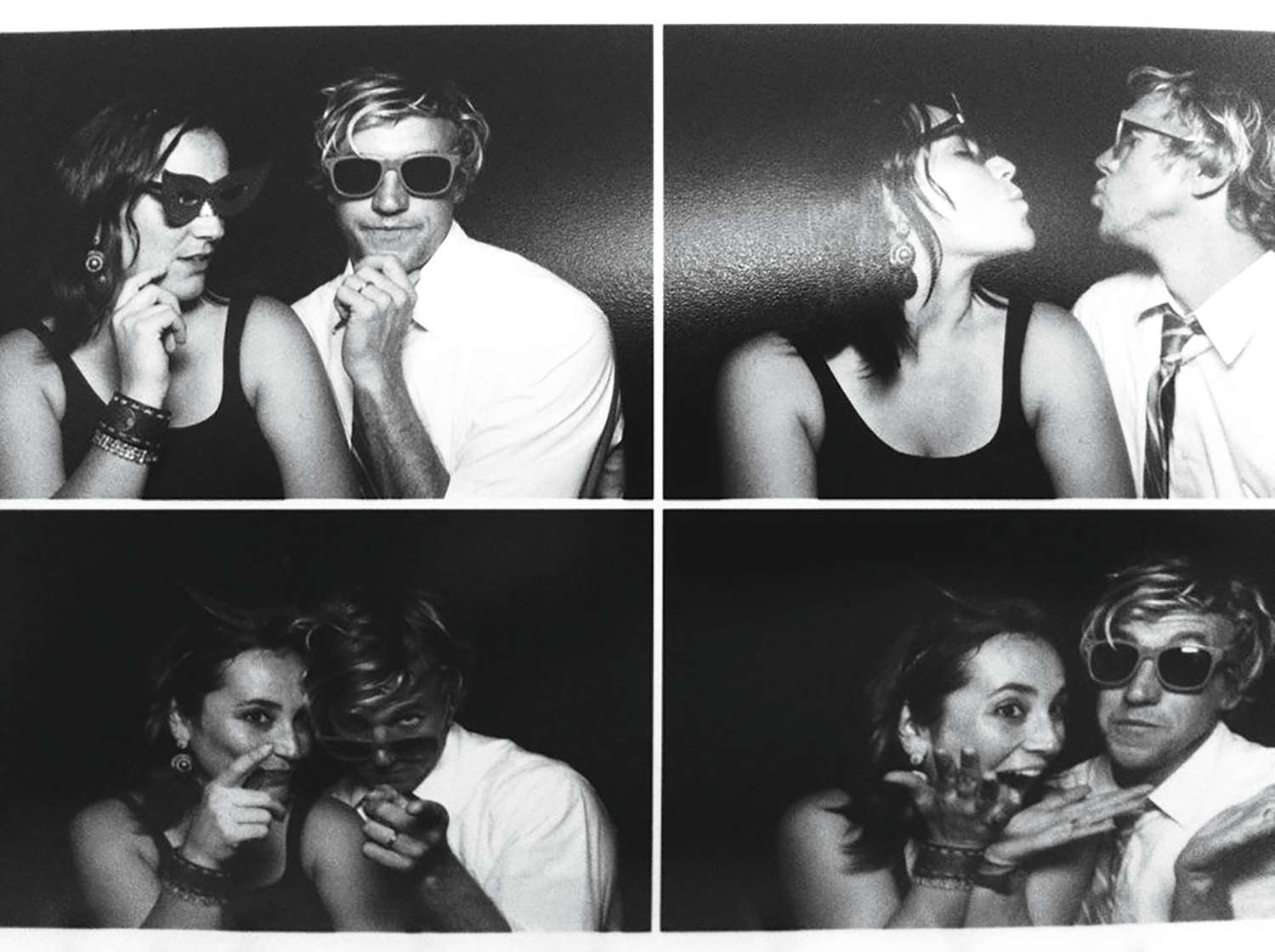
My Lovely Wife in the Psych Ward
Giulia takes a medicine dosage that seems to work without any uncomfortable side effects. But even during our best moments as husband and wife, father and mother, we can feel lingering traces of our roles as caretaker and patient. Psychiatric crises are episodic, but they cut deep into relationships and the lacerations take years to mend.
Meet Prime, the New App That Wants to Help Treat Schizophrenia
The app’s core element is a social network specially tailored to the needs of people with schizophrenia. It connects users to their peers with the illness and provides a direct line to mental-health clinicians called “coaches.” These specially trained master’s-degree-level clinicians communicate regularly with users to provide motivation and counseling in moments of need. Another feature, called “Goals,” is designed to help patients battle their motivational deficits.

The Most Dangerous Idea in Mental Health
Although there was a rapid decline in the use of memory recovery therapy and the diagnoses of multiple personality disorder, the mental health profession in the United States arguably never really came to terms with the fad that so many of its clinicians participated in—and promoted. Multiple personality disorder received a superficial facelift in the fourth edition of the DSM, released in 1994; the new moniker was “dissociative identity disorder,” but there were few changes in the diagnostic guidelines concerning the emergence of wholly separate identities in one person.

American Police and Prisons are Failing the Mentally Ill
Often, these are individuals who should have been receiving therapy for their ailments. Instead, because mental-health programs are underfunded, they end up in jail or prison for crimes—such as disorderly conduct or threatening behavior—that can be traced to their untreated illness.
To read the rest of our mental-health coverage coverage, click here.





